As We Mull Leaving Lockdown, Is Sweden Model the Way Forward?
Authored by Christina Ramirez, fist published in Real Clear Politics,
In most countries in Europe and North America, governments have imposed lockdowns of their populations and economies. At first glance, this strategy would seem to strike a reasonable, if painful, bargain: pay the price of (hopefully temporary) limits on civil liberties and economic recession (if not depression) to slow virus spread. The price has been very high. In the U.S. alone, the bill has already reached trillions of dollars of lost economic activity and tens of millions out of work. The material pain may go beyond economic insecurity. Many Americans face the real prospect of food shortages.
Sweden, however, has forged its own path. The government is emphasizing voluntary action over government mandates. Elementary schools and businesses, including bars, cafés, restaurants and gyms, are open. The government has urged people to act responsibly and follow social distancing guidelines.
Stockholm has reasoned that COVID-19 will require sustained interventions, even under optimistic timelines for the development of a vaccine. If true, the economic hardship and sacrifices to civil liberties involved in long-term societal shutdowns would become unjustifiable. So, the Swedish Public Health Authority has elected to pursue what it regards as a feasible goal of slowing the spread to prevent the overwhelming of its health care system while protecting the most vulnerable populations.
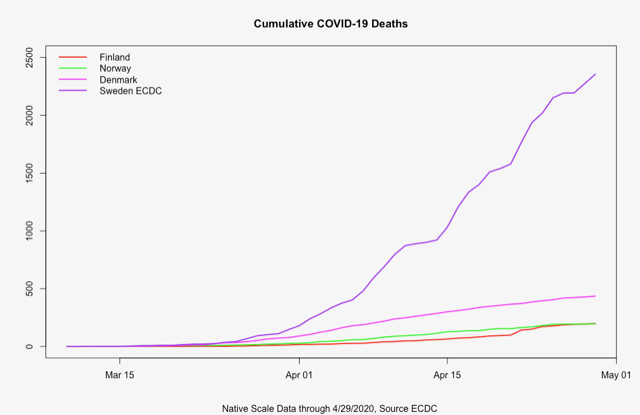
Commentators in the media have accused the Swedes of pursuing a “risky coronavirus virus strategy” or of “Russian roulette-style COVID strategy” that has caused an alarming acceleration of the pandemic, triggering a “death spike” leading to “10 times the number of deaths than its Nordic neighbors” have seen.
These commentaries seem to extrapolate too much from a narrow view of the data coming out of Sweden or are under the false impression that Sweden is not socially distancing and simply allowing the disease to spread. In fact, recent reports claiming an acceleration in COVID deaths in Sweden appear to be based on misconstruing the data at hand and narrow comparisons to other countries.
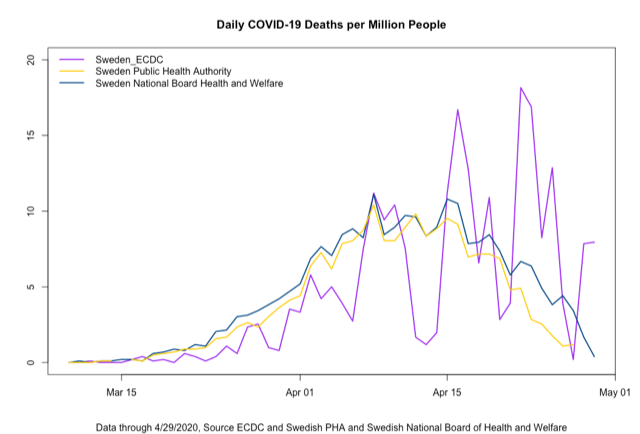
The Swedish Public Health Agency (SPHA) and the European Centre for Disease Prevention and Control (ECDC) have been reporting different daily COVID-19 death counts in Sweden. The Swedish National Board of Health and Welfare also releases COVID-19 death statistics. Although the cases reported by the SPHA and SNBHW show daily deaths on a decreasing trend, the data from the ECDC shows large swings in the death rate (Figure 1).
To understand these discrepancies, one must look into the nature of the data. The ECDC uses the day that deaths are reported. The SPHA reports the actual date of death. Using their national identification system, they report the day of death for every confirmed COVID-19 death. These numbers, unlike those in many other countries, include deaths that occur at home, nursing homes and long-term care facilities and not just those occurring at hospitals. The National Board of Health and Welfare examines the death certificates and looks for deaths that are attributable to COVID-19 and reports the date of death. Thus, they report the day of COVID-related death regardless of whether the person was tested for COVID-19 or not. It is interesting to note that roughly 4.5% of the COVID-19 deaths in the SPHA count are cases where COVID-19 was not listed as a cause of death; in other words, people died with COVID-19, not from it. Further, there are reporting delays, with weekends having lower counts and larger counts occurring later in the week. Taken together, these distinctions can paint different pictures.
Cross-country comparisons may suffer similar problems. Data cited in the press and on Twitter comparing Sweden to its Scandinavian neighbors are sometimes reported in cumulative numbers of deaths without adjusting for population size. The population of Sweden is roughly double the size of that of each of its Nordic neighbors. Such comparisons of death counts can misrepresent Sweden as a massive outlier (Figure 2).
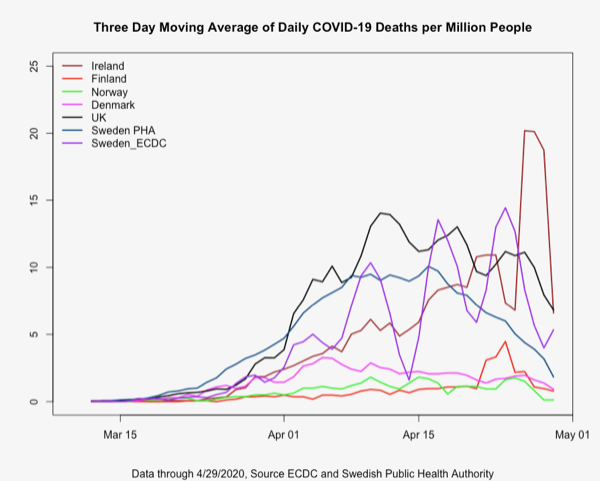
A fuller picture should bring into the comparison nearby Ireland and the United Kingdom. As daily counts can suffer from a great deal of random variability, plotting the data using a three-day rolling average of deaths per million (to account for population size differences) smooths out some of this noise and resolves the trajectory of the mortality rate into sharper focus. Appraised with this improved vision, Sweden does not appear to be such an extreme outlier (Figure 3).
Sweden represents a unique alternative as a national approach to bending the COVID-19 death curve. Perhaps as nations are contemplating relaxing their lockdowns, we should step back and take an objective, thoughtful look at what could prove to be an invaluable case study.
Stockholm trusts that people will act in their own self-interest to reduce the viral spread and, therefore, in the interest of society. This voluntary approach, however, does not exclude selective interventions and closures. While primary schools remain open to assist parents who may be health care workers and to prevent infections of elderly neighbors or grandparents who otherwise would be pressed into service as child caregivers, secondary schools and universities are closed. Visits to nursing homes are banned, and people aged over 70 have been instructed to self-isolate. Distancing is required at restaurants and gatherings larger than 50 are banned.
Judging by several indicia, Swedes are heeding the recommendations. Ridership on public transportation has dropped, working from home has increased, restaurants remain open but operate at lower capacity, and travel over the Easter holiday declined dramatically.
Sooner or later the lockdowns must end, as people become more afraid of losing their livelihood than losing their life, or as other overlooked mental and physical costs pile up to the breaking point. In the absence of effective and widespread vaccination, the viral spread can be slowed but not stopped. Singapore, for example, initially did well at containment, but now new cases are appearing. It is possible that Sweden’s larger initial wave of infection pulled forward infections that other countries are likely to encounter in subsequent waves as those nations’ lockdowns are inevitably relaxed. Indeed, Dr. Michael Ryan, executive director of the health emergencies program of the World Health Organization, suggested that perhaps Sweden “represents a future model” of what a post-lockdown society might look like .
It is too early to make definitive judgments on the relative merits and risks of the different national approaches to the COVID-19 pandemic. Furthermore, given differences in population composition, culture, health care infrastructure and other factors, successful approaches in one country or even one region might not enjoy equal effectiveness elsewhere.
But in the uncharted world of COVID-19, we must learn from all available data, including that of systems and approaches that differ from convention. Sweden has embarked upon a promising, but unproven, departure from the orthodoxy of government-ordered lockdowns. To date, Stockholm’s reliance on individual responsibility has succeeded in holding caseloads within the country’s capacity to care for the stricken. As we prepare to slowly come out of lockdown and embark for the “new normal” of tomorrow, we have lessons to learn from Sweden today.
* * *
Christina Ramirez, Ph.D., is a professor of biostatistics at the Fielding School of Public Health, University of California, Los Angeles.
Tyler Durden
Sat, 05/02/2020 – 09:20