‘Thousands’ Of Dutch COVID-19 Survivors Likely Have Permanent Lung Damage According To Top Pulmonologist
Tyler Durden
Thu, 05/28/2020 – 12:54
COVID-19 may be far less deadly than originally projected – and asymptomatic cases may be even more common than first suspected, but for those who have caught it and come down with symptoms, the disease can result in lasting symptoms, including shortness of breath, lethargy, recurrent fevers, headaches, itchiness and other mystery problems that aren’t going away.
To that end, a top pulmonologist in the Netherlands says that thousands of Dutch residents who have recovered from COVID-19 may be left with permanent lung damage, resulting in decreased lung capacity and difficulty absorbing oxygen.
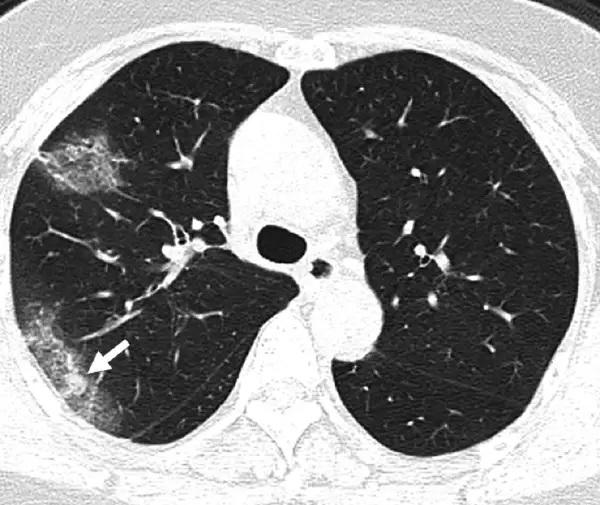
Weifang Kong and Prachi P. Agarwal
According to Leon van den Toorn, Chairman of the Dutch Association of Physicians for Pulmonary Disease and Tuberculosis NVALT, people are underestimating the consequences of the coronavirus.
“In severe cases, a kind of scar formation occurs, we call this lung fibrosis. The lungs shrink and the lung tissue becomes stiffer, making it harder to get enough oxygen,” Van den Toorn told Dutch newspaper AD (via the NL Times), adding that “there may be thousands of people in the Netherlands who suffered permanent injury to the lungs from corona.”
Of the 1,200 Covid-19 patients who so far recovered after admission to intensive care, “almost 100 percent went home with residual damage”, he said to AD. And about half of the 6 thousand people who were hospitalized, but did not need intensive care, will have symptoms for years to come.
So far 45,500 people in the Netherlands tested positive for the coronavirus. Many did not get sick enough to need hospital care. In this group, Van den Toorn expects that permanent problems will be less serious, but still possible. –NL Times
Van den Toorn says that patients experiencing lung issues should immediately see a pulmonologist, as “there may be a low oxygen level in the blood, which is harmful to the body.”
“People with a history of corona infection should be monitored closely to see if recovery is complete,” he added.
Drilling down on lung issues, let’s flash back to March, when a New Orleans respiratory therapist dealing with coronavirus patients told ProPublica that coronavirus patients suffering from acute respiratory distress syndrome (ARDS) are extremely difficult to oxygenate.
Authored by Lizzie Presser via ProPublica
“Normally, ARDS is something that happens over time as the lungs get more and more inflamed. But with this virus, it seems like it happens overnight. When you’re healthy, your lung is made up of little balloons. Like a tree is made out of a bunch of little leaves, the lung is made of little air sacs that are called the alveoli. When you breathe in, all of those little air sacs inflate, and they have capillaries in the walls, little blood vessels. The oxygen gets from the air in the lung into the blood so it can be carried around the body.
“Typically with ARDS, the lungs become inflamed. It’s like inflammation anywhere: If you have a burn on your arm, the skin around it turns red from additional blood flow. The body is sending it additional nutrients to heal. The problem is, when that happens in your lungs, fluid and extra blood starts going to the lungs. Viruses can injure cells in the walls of the alveoli, so the fluid leaks into the alveoli. A telltale sign of ARDS in an X-ray is what’s called ‘ground glass opacity,’ like an old-fashioned ground glass privacy window in a shower. And lungs look that way because fluid is white on an X-ray, so the lung looks like white ground glass, or sometimes pure white, because the lung is filled with so much fluid, displacing where the air would normally be.”
…
“It first struck me how different it was when I saw my first coronavirus patient go bad. I was like, Holy shit, this is not the flu. Watching this relatively young guy, gasping for air, pink frothy secretions coming out of his tube and out of his mouth. The ventilator should have been doing the work of breathing but he was still gasping for air, moving his mouth, moving his body, struggling. We had to restrain him. With all the coronavirus patients, we’ve had to restrain them. They really hyperventilate, really struggle to breathe. When you’re in that mindstate of struggling to breathe and delirious with fever, you don’t know when someone is trying to help you, so you’ll try to rip the breathing tube out because you feel it is choking you, but you are drowning.